What is a podiatrist?
What is a podiatrist?
Podiatrists are healthcare professionals who have been trained to diagnose and treat abnormal conditions of the feet and lower limbs.
They also prevent and correct deformity, keep people mobile and active, relieve pain and treat infections.
To become a podiatrist in Ireland you must complete a 4 year undergraduate degree in Podiatric Medicine.
At Bishopstown Podiatry Clinic we are fully qualified and experienced Podiatrists.
What is a chiropody appointment at Bishopstown Podiatry Clinic?

What is a chiropody appointment at Bishopstown Podiatry Clinic?
A chiropody appointment at the clinic refers to any nail or skin problem you may have with your feet.
The following are the most common reasons why people choose to make a chiropody appointment here:
- Nail Cutting and clean up
- Ingrown nail relief
- Removal of corns and callus
- Fungal nail infections
- Thickened nails
- Cracked heels
- Verrucae
- Athlete’s foot - fungal infection of the skin
- Blisters
What treatment is available for ingrown nails?
What treatment is available for ingrown nails?
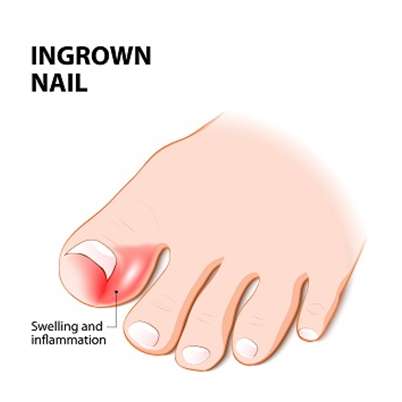
An ingrown nail is when a spicule of nail begins to pierce the skin. This can cause significant pain and lead to infections.
Risk factors for ingrown nails:
- Incorrect cutting of nails
- Tight footwear
- Adolescents
- Nail trauma
- Certain nail shapes
If you have an ingrown nail you should book an appointment with Bishopstown Podiatry Clinic and start bathing your foot in warm salty water daily and drying thoroughly until you are seen.
At the Bishopstown Podiatry Clinic, a numbing spray can be applied to help ease the pain. Then the problematic spicule of the nail will be removed gently. The area will be cleansed and dressed. At the Bishopstown Podiatry Clinic we will give you clear instructions on after treatment care and advice on how to avoid future problems with the nail.
What is a Heel Spur?
What is a Heel Spur?
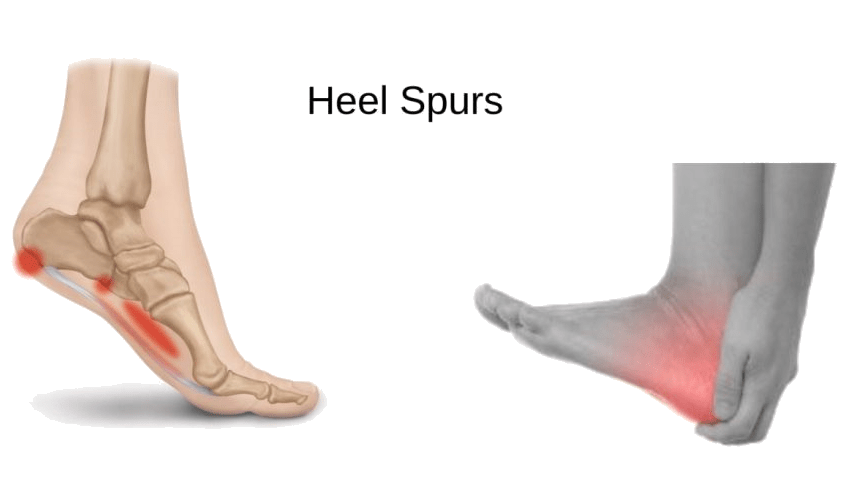
A heel spur is an abnormal growth of the heel bone. Patient’s report that the pain is often worse in the morning and the first step out of bed can cause terrible pain.
Heel spurs develop due to calcium deposits that form when the plantar fascia pulls away from the heel.
Heel spurs are commonly misdiagnosed as Plantar Fasciitis and Heel pain. It was originally thought that only 11%-16% of the population suffered with Heel Spurs but more recents studies have associated with a higher prevalence of 55% of the population.
Who develops heel spurs?
Athletes are particularly prone to developing heel spurs due to the stress placed on the plantar fascia. Any activity that causes the plantar fascia to stretch excessively can cause a heel spur to develop.
 Women also have a higher incidence of heel spurs due to the type of footwear worn on a regular basis. Flip Flops and flat shoes or slim soles provide no shock absorption.
Women also have a higher incidence of heel spurs due to the type of footwear worn on a regular basis. Flip Flops and flat shoes or slim soles provide no shock absorption.
Heel spurs are more common in people with osteoarthritis and people who are carrying extra weight as this causes more pressure on the arch of the foot to collapse.
Men and women in physically demanding jobs where heavy equipment is lifted are also prone to heel spurs due to the strain placed on the plantar fascia which then causes the fascia to pull away from the heel bone.
The body’s defence mechanism in response to trauma or excessive pressure is to deposit calcium in the heel area resulting in the heel spur. This accelerates the degeneration process of the heel bone.
 When excessive pressure is produced on the arch of the foot, this causes the foot to flatten out, causing repetitive traction of the band of plantar fascia which joins into the calcaneus (heel bone). This causes inflammation and reactive ossification (more bone material is laid down).
When excessive pressure is produced on the arch of the foot, this causes the foot to flatten out, causing repetitive traction of the band of plantar fascia which joins into the calcaneus (heel bone). This causes inflammation and reactive ossification (more bone material is laid down).
What will happen if I leave it untreated?
If the heel spur is not addressed patients may experience prolonged periods of pain and discomfort.
The heel pain may become more persistent and begin to affect you when you stand following periods of sitting down or rest.
The fat pad in the heel of the foot may start to degenerate causing increased shock transmission to the spur.
Nerve pain caused by nerve entrapment is common. The heel spur can cause abductor digiti minimi muscle to wear away, causing compression on the inferior calcaneal nerve which will produce a burning sensation in the heel.
Fracture of the spur is also common when the spur becomes enlarged.
What can help?
Stretching exercises, losing weight and wearing shoes that have a cushioned heel thatabsorbs shock can help to relieve the discomfort of a heel spur.
Elevating the heel with the use of a heel cradle, heel cup, or orthotic can also help. Heel cradles and heel cups provide extra comfort and cushion to the heel, and reduce the amount of shock and shear forces experienced from everyday activities.
What are the treatment options?
The key for the proper treatment of heel spurs is determining what is causing theexcessive stretching of the plantar fascia. When the cause is over-pronation (flat feet), an orthotic with rearfoot posting and longitudinal arch support is an effective device, and allow the condition to heal.
Along with this treatment Bishopstown Podiatry Clinic will also provide personalised strengthening exercises to build up the muscles which hold arch of the foot. Orthotics may be prescribed for a short period of time to help alleviate the pain and support the muscles.
What causes flat feet in adults?
What causes flat feet in adults
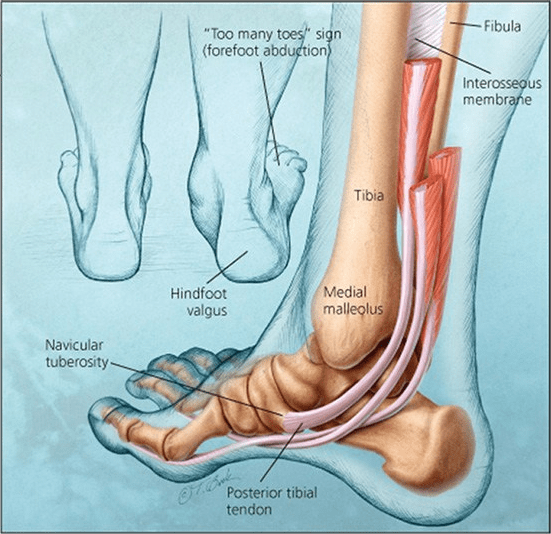
Believe it or not there are different types of flat feet, thats why some people may find different shoes and orthotics comfortable but someone else may find that they blister or even make the pain a lot worse.
Flat feet also known as Pes Planus, can occur with mobile feet, rigid feet, after trauma like an ankle break or even surgery.

Most common cause of flat feet in adults that I see in clinic every day is Post Tibial Tendon Dysfunction, sometimes referred to as Adult-acquired flat foot. This is where the tendon holding up the foot looses its strength and the foot collapses. It causes the arch of the foot to over pronate, and this in turn places strain on the ligaments and tendons in the ankle and sole of the foot.
A tight Achilles tendon can appear to make the foot look flat. When the achilles is too tight, the biomechanics of how we walk change causing the foot to roll inwards, inducing pain on the achilles and the heel.
Pregnancy can also cause the feet to flatten. In the third trimester when your body prepares for the delivery of the baby, there is increased elastin (elasticity) in the body, this combined with the extra weight of the baby caused the tendons to lose their strength and the foot collapses.
Symptoms of Flat Feet
Flat feet can be extremely debilitating if left untreated. We usually see patients attending clinic as a last resort when they’ve tried all the pharmacy insoles, specialist shoes and even taken time of work to just rest.
 Flat feet can cause pain in the foot, arches, heels, calves, shins and even the knees and hips. More recent studies have suggested a correlation between flat feet and migraines.
Flat feet can cause pain in the foot, arches, heels, calves, shins and even the knees and hips. More recent studies have suggested a correlation between flat feet and migraines.
Pain can radiate through-out the day, but most often it occurs first thing in the morning or after periods of sitting. The arches of the foot can appear swollen or puffy from inflammation of the tendons and muscles.
Treatment
Treatment of flat feet is simple once the cause of the pain is established. At Bishopstown Podiatry Clinic we carry out a full biomechanical gait analysis.
Treatment will include:
- Correct diagnosis and severity of the condition.
- Exercises that can be carried out at home
- Recommendations for footwear
- Manual therapy such as dry needling or tissue mobilisation maybe required with some patients.
- Custom orthotics provide the best support for the treatment of flat feet as they are prescribed to the exact mechanics of your feet. These can be claimed against most major insurance companies.
- Goal setting is also a major part of our consultations so that we can get you back to your daily activities and hobbies immediately.
What are Chilblains?
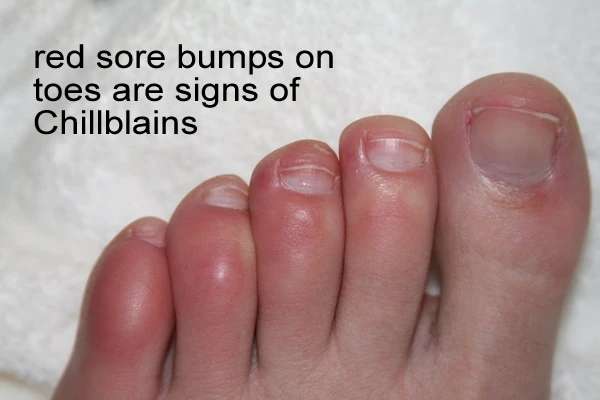
What are Chilblains?
Chilblains affect the toes but can also affect the fingers, ears and nose. They appear on the skin as small, itchy swellings which occur from exposure to cold temperatures and damp environments.
The medical term for Chilblains is Pernio, which is an inflammatory skin disorder. They can be painful but rarely cause any permanent damage. They will normally heal within a couple of weeks if further exposure to the cold is avoided.
Symptoms of Chilblains
- A burning sensation in the hands and feet
- Blue, red or white swollen patches on the skin
- Extreme sense of wanting to scratch the area
- Dry skin – leading to cracks and wounds
- Ulcers
- Infection
What causes it?
The majority of sufferers develop Chilblains in the winter due to the low temperatures. They are especially common in the Ireland because of damp and cold weather conditions during the winter months.
Chilblains are more common in women and also in people who suffer from hyperhidrosis (excessive sweating) and low body mass index.
The low temperatures cause a restriction of a small branch of artery leading to the capillaries which supply blood to the skin. When the skin is warmed quickly, this can lead to blistering, redness and itchy lesions. It is best to avoid going straight to a heater or a hot water bottle – warm up your feet gradually!
 If you suffer from poor circulation or if you work in an environment where you are regularly exposed to cold and damp conditions you may be more likely to develop Chilblains.
If you suffer from poor circulation or if you work in an environment where you are regularly exposed to cold and damp conditions you may be more likely to develop Chilblains.
In the majority of cases, symptoms will resolve in 1-3 weeks. If symptoms persist and become chronic, it may indicate underlying conditions such as Systemic Lupus Erythematosus, Sarcoidosis or Raynaud’s Phenomenon.
What will happen if I leave it?
Chilblains usually don’t require any treatment as the symptoms often get better on their own after a week or two.
It is common for Chilblains to reoccur or become severe which puts you at risk of developing further problems. If the itchy area of the skin becomes broken, it is common for infections to occurs. In the most severe cases, ulcers may develop on the skin which can cause pain when moving
To avoid complications such as these it is advisable not to directly overheat the area and to try to refrain from itching or scratching the skin.
What can help?
If you do suffer from Chilblains you can reduce your risk of developing them by limiting your exposure to cold environments.
If your feet do get cold,
- Warm them up gradually as heating them too quickly is one of the main causes of Chilblains.
- Wear 100% cotton socks or Bamboo socks have been proving beneficial as they reduce bacteria and absorb moisture from the skin- keeping your feet drier.
- Do not scratch the skin.
- Regulating moisturising your feet and massaging them to keep the soft and warn and preventing the skin from splitting.
- Lanolin cream soothes the cracks and itch that can occur from chilblains.
- Warming your shoes and slippers on the radiator before you put them on.
- Do not heat your feet or hands near heaters or fires.
- Do gentle exercises to warm up your feet before going out – like jumping on the spot, this will improve circulation.
What are the treatment options?
If the skin is itchy, a soothing lotion such as witch hazel or calamine can help. Most importantly, keeping the toes warm and dry as much as possible. Occasionally the skin can break. If it does, apply a dressing to keep infection at bay. A combination of a healthy diet and regular exercise have also been proven to reduce the occurrence of Chilblains.
If you think you may have an infection or symptoms are not improving it is important to seek treatment as soon as possible. At Bishopstown Podiatry Clinic we will be able to diagnosis correctly, apply dressings and prescribe creams which will improve the condition.
What is Achilles Tendinopathy?
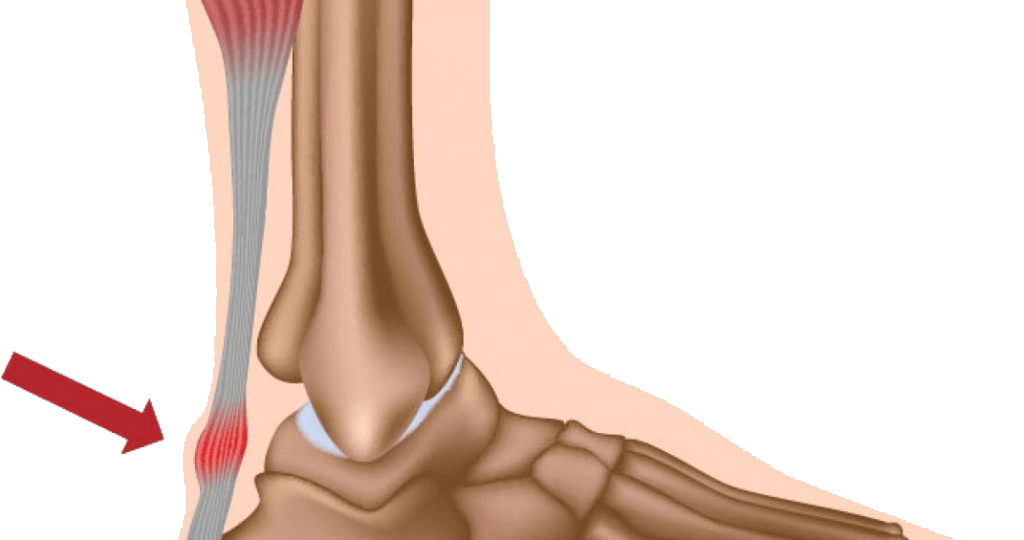
What is Achilles Tendinopathy?
You may have heard of different terms for Achilles Tendonitis. Achilles Tendonitis is Latin for ‘inflammation of the Achilles Tendon’. Tendinopathy refers to the disease of the tendon if the inflammation is not present.

Achilles Tendons are the longest tendons in the body, connecting the calf muscles to the heel bone. When the calf muscles contract, they pull on the Achilles Tendon, causing the foot to point down and helping you rise on your tiptoes.
It is one of the most common injuries in athletes, estimating to afflict up to 20% of all runners.
Achilles Pain occurs just above the back of the heel and often you will also experience tightness in the calf muscles. Pain is present with walking and running, especially when pushing off on the toes.
What causes it?
Achilles Tendonitis pain can develop gradually without any history of injury or trauma. The pain can be a burning pain, a shooting pain, or even an extremely piercing pain.
Achilles Tendonitis should not be left untreated because there’s a chance the tendon will become weak and ruptured.
Achilles pain can be aggravated by activities that repeatedly put stress on the tendon, causing irritation and inflammation.
The most common reported cause of Achilles Tendinopathy is repetitive load which exceeds the ability of the tendon. This can be caused by tight calf muscles, excessive pronation (flat feet) or limb length discrepancy (one leg longer than the other).
Other causes include long distance marathon running, where the tendon is constantly under extreme stress undertaking different terrains, hill running, running on uneven terrains and hard surfaces. This causes the tendon-muscle unit to change traction too quickly.Are your running shoes showing excessive wear patterns on the outer sole? Or the heel of the shoe distorted where you are landing unevenly ? Lower limb malalignments such as:
- Tibial Varum (bowed legs)
- Compensated Gastroc-soleus Equinus (limited flexibility in the calves)
- Ankle Block Equinus (limited movement in the ankles)
- Cavus Foot Type (high arched foot)
- Hyperpronation (foot rolling inwards too much when the foot lands to the ground)
All theses conditions will be checked by your Podiatrist during a comprehensive Biomechanical Assessment.
During the assessment we will check the flexibility of hamstrings, quadriceps and calf muscles. Bring along your running shoes and shoes you wear most often to check for wearing patterns.
From our OptoGait system we will analyse and video your Gait (walking pattern) and show you how you can further improve your run to prevent problems occurring in the future and provide an individualised recovery plan.
Achilles pain is a common problem, and often experienced by athletes, particularly distance runners.
Achilles Tendinopathy is a difficult injury to treat in athletes due to their high level of activity and reluctance to stop or slow down their training.
Persistent strain on the Achilles Tendons causes irritation and inflammation. In severe cases this strain may even cause the tendon to rupture!
Chronic overuse (particularly in runners) may contribute to changes in the Achilles tendon as well, leading to degeneration and thickening of the tendon.
What will happen if I leave it untreated?
Achilles Tendonitis can develop into a chronic condition if left untreated. The risk of a tendon rupture is also increased. Movement can also become restricted if untreated and if you continue with the activity that has caused the injury.
What can help?
Rest, ice, exercises and NSAID’s such as ibuprofen can help to relieve the symptoms.
It is vital to stop the activity that has caused your Achilles pain as soon as it happens. This will prevent any further damage and will allow the tendon time to heal. Rest is aimportant part of the recovery process.
 You can start to gently introduce activity as the pain decreases but if you feel pain you should stop immediately and rest. Applying ice to the painful area can help to reduce inflammation. Do not apply ice directly to the skin. Wrap in a towel and apply to the affected area for 10-20 minutes three times a day.
You can start to gently introduce activity as the pain decreases but if you feel pain you should stop immediately and rest. Applying ice to the painful area can help to reduce inflammation. Do not apply ice directly to the skin. Wrap in a towel and apply to the affected area for 10-20 minutes three times a day.
At Bishopstown Podiatry Clinic we will correctly diagnose your condition and start you on a treatment a rehab programme which may include taping & strapping, soft tissue mobilisation, dry needling, manual stretching, orthotics, or a stretching and strengthening plan to take home with you.
What is nail reconstruction?

What is nail reconstruction?
At Bishopstown Podiatry Clinic we can reconstruct your nail with a medical grade nail. It feels, looks and behaves like a real nail. The medical nail can be cut and filed like a real nail. The nail has a lifespan of 2-3 months. People who opt for this treatment are usually tired of hiding their damaged nails.
How do you treat fungal nail infections?

How do you treat fungal nail infections?
Firstly, the nail is cleaned and all diseased nail is removed. An antifungal agent is applied to the nail and home treatment is advised.
At Bishopstown Podiatry CLinic we ensure that the procedure is very effective and pain free.
What is an orthotic?
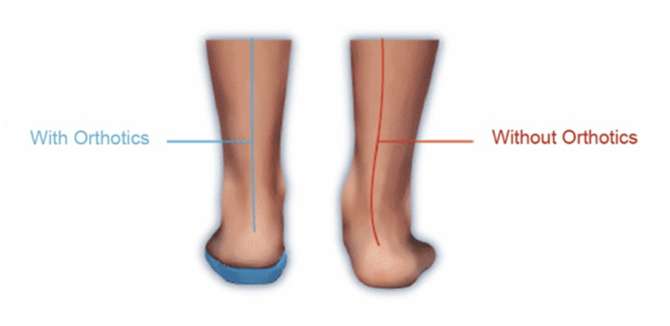
What is an orthotic?
An orthotic is a customised insoles that redistributes the forces in your feet so you can walk pain free again.
At Bishopstown Podiatry Clinic all customised orthotics are made in one of Europe’s leading manufacturers in custom orthotics.
What is plantar fasciitis?

What is plantar fasciitis?
Plantar fasciitis is the most common cause of heel pain. Most patients will describe the pain as being at its worst first thing in the morning. The plantar fascia is a large ligament at the bottom of your foot. Its insertion point is at your heel bone. This point of insertion can become inflamed and painful. There are a number of factors that put you at risk of developing this condition.
- Tight muscles
- Weak muscles
- Abnormal foot mechanics
- Poor footwear
- Prolonged standing
- High BMI
- Leg length discrepancy
The good news is this condition is very treatable. If you are experiencing heel pain, make an appointment today to see a qualified podiatrist at Bishopstown Podiatry Clinic.
How does diabetes affect your feet?
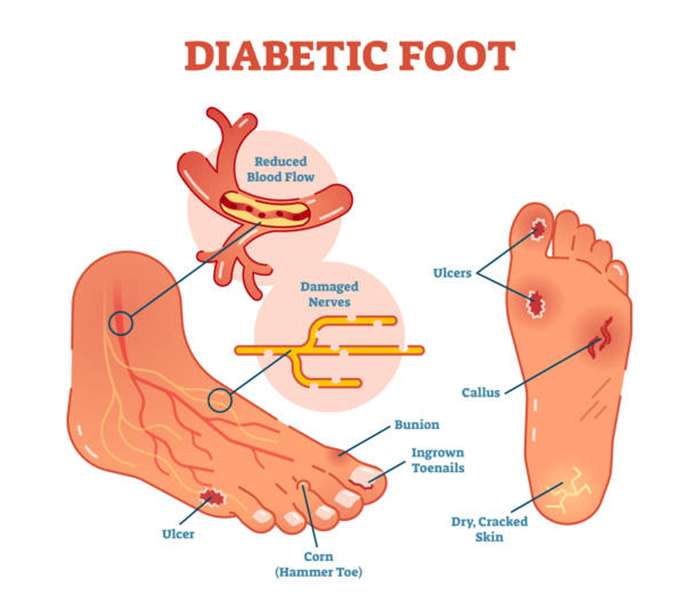
How does diabetes affect your feet?
Over time high blood sugars can cause damage to blood vessels and nerves. This results in loss of normal blood flow and sensations to your feet. It is important to have regular foot checks from your podiatrist to monitor this.
Reduced blood flow and lack of sensation puts you at risk of developing ulcers (non-healing wounds), infections and amputations. At Bishopstown Podiatry Clinic we recommend regular visits to one of our podiatrists to significantly decrease your risk of developing diabetic foot disease.
What is a verruca?

What is a verruca?
A verruca is a benign form of the human papilloma virus (HPV). HPV creates a lesion on your skin. Typically they appear as a white mass with black spotting.
You are most at risk at contracting a verruca in public swimming pools, changing rooms and from skin to skin contact. Verrucae typically spread in warm moist environments where you are barefoot. Always remember to wear flip flops in public changing rooms and pools!
If you think you may have a verruca and are looking to have it treated, you can book a consultation here at Bishopstown Podiatry Clinic.
What is the conservative treatment available for bunions/hallux valgus?
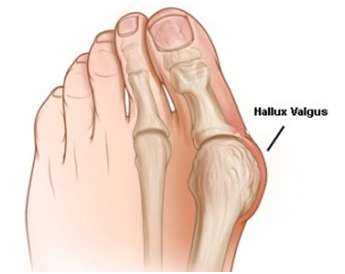
What is the conservative treatment available for bunions/hallux valgus?
A bunion is a structural change to your big toe joint causing a deformity to the foot. The medical term for this is hallux valgus. Essentially, what has happened to your foot is a dislocation at your 1st metatarsophalangeal joint (at the base of your big toe). This results in the toe deviating towards your lesser digits and the metatarsal bone deviating towards your midline. It is a progressive condition, therefore over time the deformity becomes more pronounced.
This is a very common foot condition in the population. It affects women more than men. It is estimated that as many as 50% of women in the population have a hallux valgus.
For many individuals, they do not experience pain in their feet with a hallux valgus. Their biggest issue is finding accommodative footwear. However, if you are experiencing pain, there are a number of conservative treatments available to keep you pain free and avoid going down the surgery route. Conservatives interventions can also slow the progress of the hallux valgus.
Conservative interventions include:
- Orthotics/ custom insoles
- Exercises
- Stretching and strengthening
- Chiropody care
- Footwear
What treatments are available for nerve entrapment conditions in the foot?
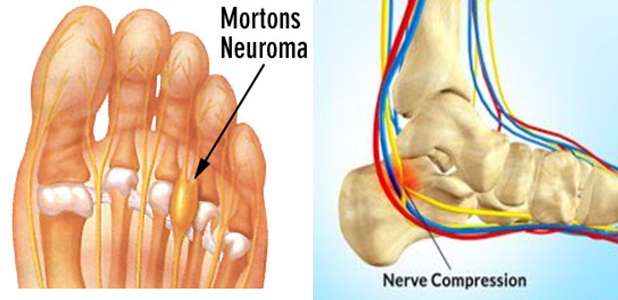
What treatments are available for nerve entrapment conditions in the foot?
The most common nerve entrapment conditions in the foot are Baxter’s nerve entrapment (located at the heel) and Morton’s neuroma (in the forefoot).
Symptoms associated with a nerve entrapment are sharp shooting pains, burning sensations and/or numbness.
This condition is a result of nerve compression and irritation. The outer sheath of the nerve reacts to the compressive forces by enlarging. The most common causes of a nerve entrapment are:
- Foot mechanics
- Tight and/or weak muscles
- New activity
- Footwear
At Bishopstown Podiatry Clinic we can treat this condition, a biomechanical assessment must be performed to identify the leading cause of the pain.
Based on this information a rehabilitation plan will be formed. Such plans may include orthotic therapy and exercises.
