Every 30s someone loses a limb to diabetes according the American Association of Diabetes. It is the leading cause of amputation globally. This is a preventable outcome. You can reduce your risk of lower limb amputation significantly by visiting your podiatrist annually.
Diabetes is a disease that is caused by an insufficiency, or lack of insulin in the body. Insulin allows sugar (or glucose) to enter cells and when there is a reduction in insulin, the sugar has nowhere to go. As the sugar can’t enter the cells, it collects in the bloodstream, creating ‘high blood sugar (glucose) levels’.
There are two types of diabetes:
Type 1 – The body’s immune system destroys insulin-making (beta) cells in the pancreas and so no insulin is produced. This occurs mainly in childhood or early adulthood.
Type 2 – The pancreas does not produce enough insulin or struggles to effectively use the insulin it does produce and thus cannot control blood sugar levels.
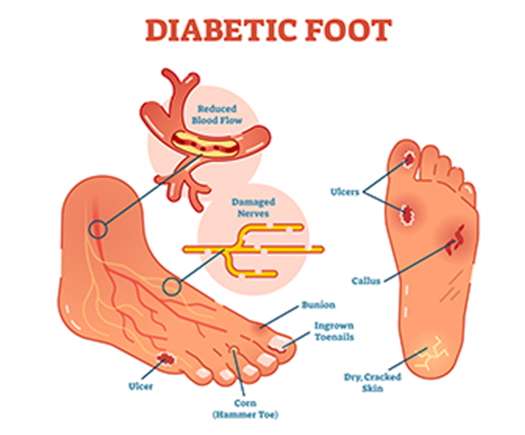
If poorly managed, diabetes can cause secondary health problems, many of which affect the feet
Diabetes Effect on your Eyesight – Diabetic Retinopathy:
High blood sugar levels can cause damage to the retina (the back of the eye), which can cause impaired or total sight loss. This makes it very difficult to look after one’s own feet, you will be more likely to cut yourself as you cannot see exactly what you are doing.
Diabetes Effect on your Circulation – Peripheral Vascular Disease (PVD):
PVD is a slow and progressive circulation disorder that affects arteries, veins and lymph vessels and occurs as a result of a narrowing or blockage in the blood vessels. In this case the sugar builds up in the vessels and creates a blockage. This means that there is reduced blood supply reaching the body’s extremities such as the hands and feet, creating a poor healing environment which can cause a simple cut to develop into an ulcer and lead to amputation.
Diabetes Effect on your Nervous System

– Sensory Neuropathy:
Patients with diabetes are at a higher risk for cuts and abrasions as sensation in the feet may become diminished. This can occur from a condition called peripheral neuropathy which causes damage to the nerves from poor circulation occurring in the extremities such as the feet. The nerves become damaged and fire incorrect signals to the brain, creating altered sensations of numbness or sharp, burning pain. If you are experiencing peripheral neuropathy you may not notice a cut or blister to your foot as you do not have pain receptors.
– Motor Neuropathy:
If your blood sugars remain high over long periods of time, the muscles in your lower limbs can become small and weaker. This changes the shape of your foot, you lose some of the range of movement in your ankles, your arch becomes higher and your toes begin to claw. This creates high areas of pressure that can lead to ulcerations.
– Proprioception:
Proprioception is the body’s ability to detect where in is in your surroundings, it is another word for balance. Diabetes can lead to poor balance and changes in the way you walk. This increases your risk of falls.
– Charcot Foot:
Diabetic Peripheral Neuropathy can lead to damage to the feet, as you may not notice injured or broken bones. Because of the neuropathy, you will be able to walk without pain, but as you put pressure onto the foot it can start to alter the shape of your foot. This leads to a misshapen foot, which puts you at a greater risk of developing a diabetic foot ulcer.
Some things you can do to look after your overall and foot health:
- Visit your podiatrist every 6 months for diabetic assessments and routine care. Seeing a podiatrist annually can decrease your risk of amputation significantly.
- Check your feet daily to make sure that there are no cuts or abrasions you are unaware of. If there is a cut or abrasion that is not healing, notify your GP and schedule an appointment with your podiatrist.
- Check your footwear daily. Ensure that there are no stones or obstructions lying in the shoes that you may not feel due to sensation loss.
- Wear comfortable, supportive footwear with a wide toe box and laces or Velcro to ensure your feet aren’t sliding around. Assess the need for replacement of footwear on a yearly basis.
- Avoid placing your bare feet in public spaces such as the gym, swimming pool or hotel bathrooms as it can be easy to contract a fungal nail infection, athlete’s foot or a verruca. Verruca socks or flip flops are a handy solution for unlicensed environments.
- Use moisturiser every day to keep the feet from getting dry and cracked. Do not apply cream between the toes as the area can become warm and moist, attracting fungal bacteria and creating problems such as athletes foot and fungal nail infections.
- Do not use blades or corn plasters on your feet, as this may cause symptoms to worsen. Contact your podiatrist for advice if you are unsure.
- Look after your own health, including sugar levels, diet, exercise and smoking habits. For further advice regarding this, contact your GP or dietician.
What to expect at your appointment with the Podiatrist:

- We will go through a full history take at your first appointment such as asking questions like: when were you diagnosed? What are your most recent blood sugars like? Have you had any previous complications with your feet, such as surgeries, ulcers, or amputations?
- Make sure to bring a list of medication you are taking or any other medical conditions you may have.
- We will use a doppler to check your circulation. A doppler is a small machine that listens to the two main arteries in your feet, the dorsalis pedis pulse and the posterior tibial pulse.
- We will use a monofilament to check the sensation in your feet. It is a small instrument that applies light pressure to different areas of the foot. From carrying out this test we can assess what level of nerve damage, if any, may be present in the feet.
- We will use a Neurotip to test your sensation of pain. This involves using an instrument with a sharp end and a blunt end and you will be asked to decide if what you feel is sharp or blunt.
- We will use a tuning fork to assess your sensitive of vibration. Due to nerve damage and ageing, sensation of vibration can become diminished and this instrument creates a vibration that is applied to the bony prominences of the feet. You will be asked if you can feel this vibration or not.
- We will carry out proprioception tests to test your awareness of your surroundings, it can be altered due to nerve damage and makes you more susceptible to hurting yourself by bumping into things or falling.
- We will carry out routine chiropody care such as cutting your nails, removing corns or callus that may be present.
General Advice:
When coming to your podiatry appointments, bringing the shoes you wear on a day-to-day basis lets the podiatrist assess your footwear and see if they’re suitable for you. If your issue is associated with walking or exercise, please bring your exercise shoes. If you own a pair of orthotics, bring those along too! We advise that you wear shoes that are easy to take on and off. We also apply an emollient or cream following your treatment and so socks and supportive shoes would prevent slipping and sliding on the drive or walk home.
Bishopstown Podiatry Clinic prides itself for providing exemplary podiatry care for all patients who attend and following this guide can help your podiatrist provide the best and most suitable treatment for your specific needs. If you have any concerns or queries regarding your first appointment at our clinic, please don’t hesitate to email us at info@bishopstownpodiatryclinic.com
We look forward to meeting you!
Click to make an appointment by phone: 021-4867629Click to make an online appointment

Leave a Reply